The impact of smoking on all aspects of health – physical, psychological and socioeconomic – is so serious that helping people to quit is a key priority for anyone working to improve health outcomes. In this article, we look at the best way to encourage smokers to quit, how to increase the quit rate in smokers who have decided that the time is right for them to stop, and review the latest information on pharmacological options for smoking cessation.
Raising the issue with patients: let’s talk about sex
The quality of many of our patients’ lives would improve if they had the choice and ability to be sexually intimate. It is relatively common for men who suffer from cardiovascular disease or diabetes to suffer from erectile dysfunction (ED). They often feel too ashamed to initiate sex with their partner, or start a new relationship, because they are unable to gain or maintain an erection. They can become socially isolated and aviod physical contact. As healthcare professionals, we owe this group of patients an opportunity to talk about their sexual problems and to offer them support and treatments. But how do we open up a discussion about sex?
Motivating women and men: what presses the right buttons?
Getting people to act on advice is a continuing challenge for health professionals, particularly in the self-management of chronic conditions. In this article, we explore why men are less likely than women to fully engage with their own health needs and what health professionals can do to help men get better at this. Using the behavioural theory of communication – the Theory of Primitive Concerns – we will look at how different responses to risk – with women typically being risk-averse and men being risk-seeking – mean they respond differently to two alternative styles of clinical instruction based on using ‘power language’ and ‘safety language’. The theory is that we can help men to look after their own health by using language that matches their attitude to risk and presents self-care in a more powerful way.
Editorial
Keep up the good work’ is the theme of this issue of BJPCN, with latest figures showing that the structured care we provide to our patients is helping to save lives. But we are not there yet – so we are looking at remaining challenges in managing cardiovascular disease and what more we can do to really make a difference to our patients’ lives.
The ultimate cholesterol lowering plan step-by-step
In the last two issues of BJPCN, we have provided you with the scientific evidence for the Ultimate Cholesterol Lowering Plan (UCLP) and how its impressive cholesterol-lowering impact can help save lives from coronary heart disease and reduce the £3.3 billion financial burden to the NHS.1 In this issue, we discuss how you can apply the UCLP in your day-to-day practice to bring about clinically significant cholesterol-lowering results for all your patients.
Editorial
Chronic kidney disease (CKD) has shot up the primary care agenda over the last few years, and is now well recognised as an independent risk factor for cardiovascular disease (CVD). At the same time, CVD is a risk factor for progression of CKD. The close links between CKD and CVD mean we have to get to grips with assessing patients’ kidney function and ensuring those with CKD receive the treatment needed to prevent progression. This special issue devoted to CKD is full of step-by-step guides and illustrated articles to help you get to grips with this important condition.
Editorial
The effective management of long-term conditions such as chronic kidney disease (CKD) is probably the single greatest challenge faced by the NHS. The population is growing and people are living longer. Every week, the life expectancy for a newborn baby in the UK increases by more than 24 hours. While this is, in part, testament to the success of our health services, it also places steadily increasing demands upon them. As the population ages, the number of people living with long-term conditions is predicted to triple by 2050.
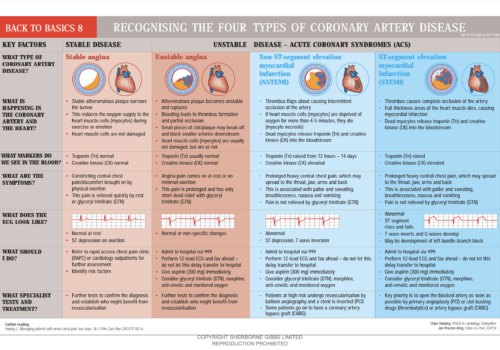
Back to Basics: Recognising the four types of coronary artery disease
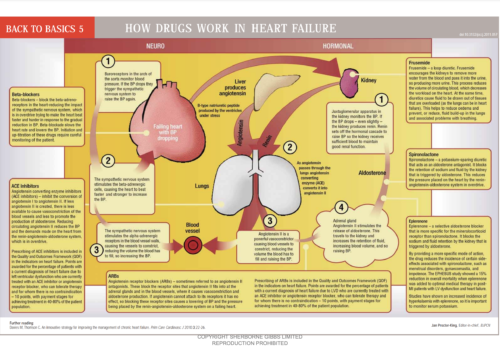
Back to Basics: How drugs work in heart failure
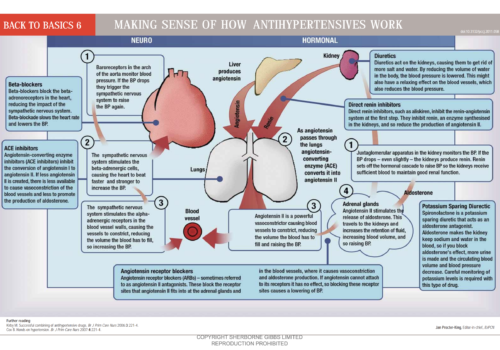
Back to Basics: Making sense of how antihypertensives work
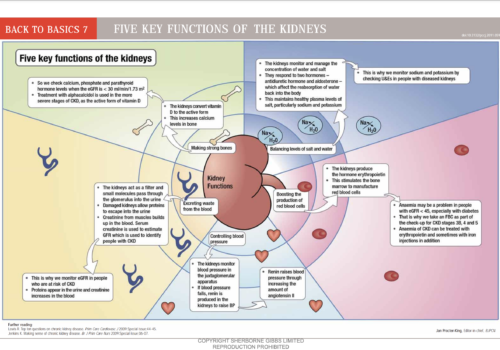
Back to Basics: Five key functions of the kidneys
Understanding end-of-life care in advanced kidney disease
People with advanced kidney disease are required to make many choices about their treatment throughout the journey of this disease. Opting not to have dialysis or to withdraw from treatment is a difficult decision and there are many factors that influence patients’ decisions. For those who choose not to have dialysis, the implications need to be understood by the patient, their family and carers and healthcare professionals involved in their care. This article provides an update on this important issue to equip primary care professionals with a clear understanding of end-of-life care for patients with advanced kidney disease.