There are several different drug types used in the management of hypertension. This back to basics provides a useful summary of the different antihypertensive drug classes and how they act to regulate blood pressure.

This resource is fully searchable using the search box at the top of the page, or to narrow down your selection using filters click on 'Knowledge hub' in the main navigation.


People with COPD should be reviewed at least annually according to the Quality and Outcomes Framework. However, there is little mention of the importance of assessing nutritional status and no ‘QOF’ points for doing so. This article describes the assessment and management of COPD patients with a risk of malnutrition.
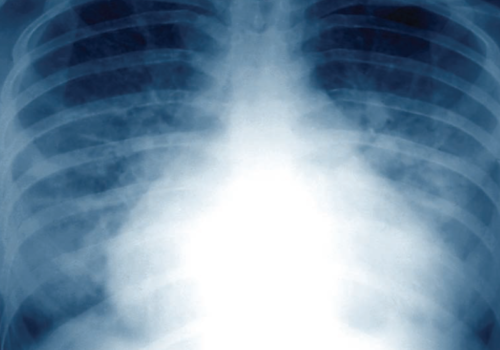
Heart failure is characterised by fatigue, breathlessness and retention of fluid. The update of the National Institute for Health and Clinical Excellence chronic heart failure guidelines has simplified its management by using a stepped approach to investigation and treatment. In this article, we focus on the practical aspects of managing the two main symptoms associated with heart failure – oedema and breathlessness.

Chronic obstructive pulmonary disease (COPD) is a largely preventable, slowly progressive, inflammatory disease. Rates of COPD are rising faster in women than in men, yet women are less likely to be diagnosed. There is currently no cure, but best-practice management outlined in recently updated NICE guidelines can help to improve patients’ symptoms and quality of life.

Chronic clinical conditions have traditionally been regarded as individual disease categories within individual patients, although there is often considerable overlap across clinical systems. However, for those managing these patients the presence of various co-morbidities is all-too apparent. It may be time to consider a new approach to management of these patients.
Cardiovascular morbidity and mortality in patients with chronic obstructive pulmonary disease (COPD) is nearly double the rate in the general population without COPD. And for those with cardiovascular disease (CVD) and COPD, heart failure is the most common cause of hospitalisation.
Chronic clinical conditions have traditionally been regarded as individual disease categories within individual patients, although there is often considerable overlap across clinical systems. The monitoring of patients with long-term conditions has historically centred around a traditional model of a nurse-led clinic, utilising an appropriate level of skill mix. The disease categories and associated clinical indicators of the Quality and Outcomes Framework (QOF) have encouraged this approach, but for those managing these patients the presence of various co-morbidities is all too apparent
The Department of Health’s Expert Patient Programme recognises the role of selfmanagement
in many different disease areas and its report Self Care recommends the
concept of encouraging people with long-term conditions to self-manage where
possible. Diabetes management would never succeed without the active participation of
the person with the condition and asthma management plans have been advocated for some
time for people with asthma. What can self-management plans achieve in chronic obstructive
pulmonary disease (COPD)?
Cough as a symptom results in significant impairment of quality of life for patients. Its
wide and varied causes and presentations make diagnosis and management complex.
Many sets of guidelines have been produced to help clinicians in the evaluation and
management of acute and chronic cough. This article uses the British Thoracic Society
(2006) guidelines to provide a summary of the evaluation and management of cough.
A unique new e-platform for primary care

For healthcare professionals in countries with applicable health authority product registrations. The content may not be approved for use in your specific region or country. Please review the applicable product labelling for your country for indications and instructions prior to use. If not approved, please exit this site.
We use cookies to ensure that we give you the best experience on our website.
By continuing to this site you are confirming that you are a healthcare professional and are opting into the use of cookies.


















