The effective management of long-term conditions such as chronic kidney disease (CKD) is probably the single greatest challenge faced by the NHS. The population is growing and people are living longer. Every week, the life expectancy for a newborn baby in the UK increases by more than 24 hours. While this is, in part, testament to the success of our health services, it also places steadily increasing demands upon them. As the population ages, the number of people living with long-term conditions is predicted to triple by 2050.
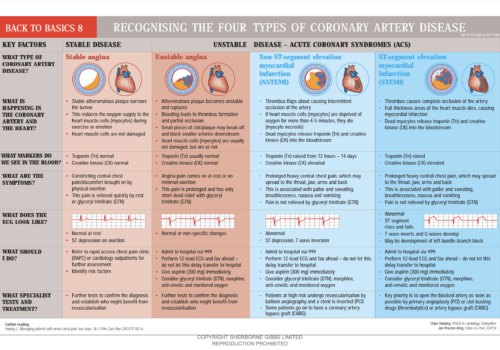
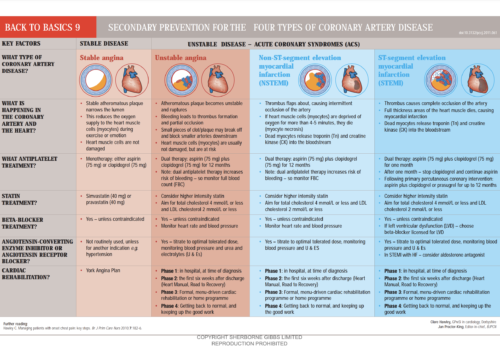
Back to Basics: Recognising the four types of coronary artery disease
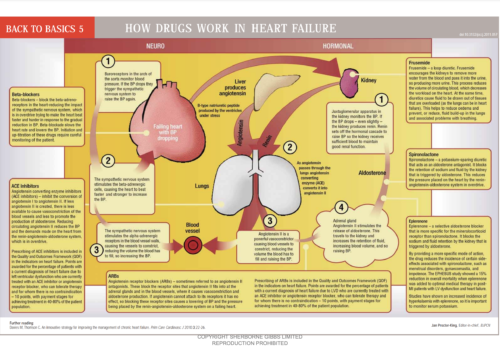
Back to Basics: How drugs work in heart failure
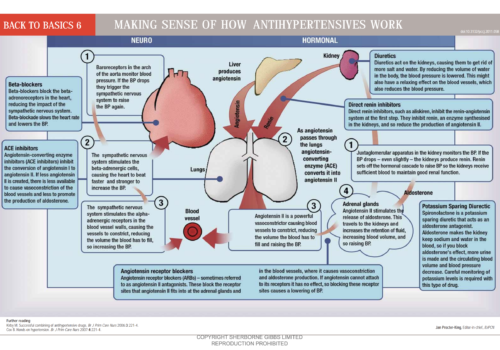
Back to Basics: Making sense of how antihypertensives work
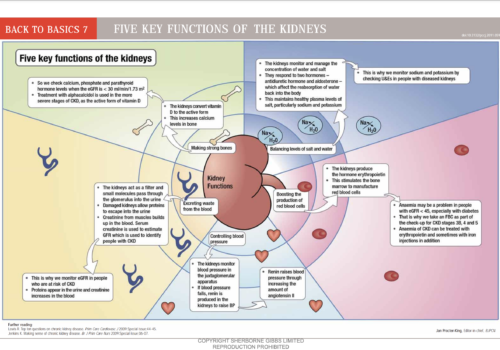
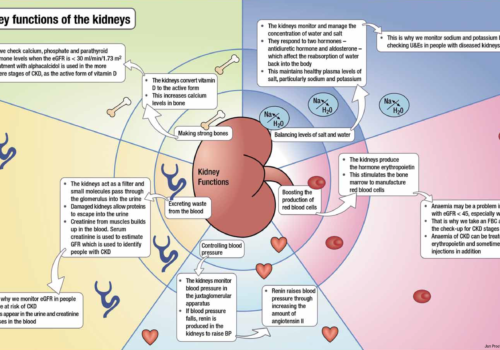
Back to Basics: Five key functions of the kidneys
Understanding end-of-life care in advanced kidney disease
People with advanced kidney disease are required to make many choices about their treatment throughout the journey of this disease. Opting not to have dialysis or to withdraw from treatment is a difficult decision and there are many factors that influence patients’ decisions. For those who choose not to have dialysis, the implications need to be understood by the patient, their family and carers and healthcare professionals involved in their care. This article provides an update on this important issue to equip primary care professionals with a clear understanding of end-of-life care for patients with advanced kidney disease.
Making sense of chronic kidney disease
What exactly is chronic kidney disease (CKD), what causes it and how is it diagnosed? In this article we get down to the basics of defining what CKD is, and explore the stages of CKD. We review CKD progression and the assessment and management recommendations for each stage of CKD.
Kidney damage and what it means to you
Back to Basics: Secondary prevention for the four types of coronary artery disease
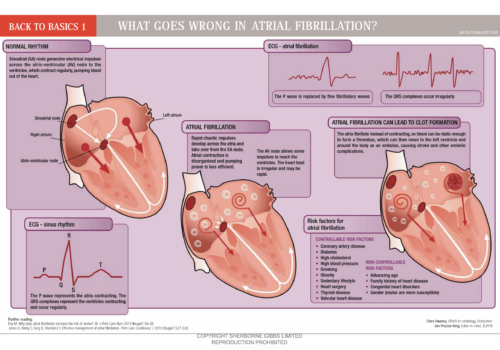
Back to Basics: What goes wrong in atrial fibrillation (updated September 2011)
A primary care guide to chronic kidney disease
Chronic kidney disease (CKD) has shot up the primary care agenda over the last few years, and is now well recognised as an independent risk factor for cardiovascular disease (CVD). At the same time, CVD is a risk factor for progression of CKD. The close links between CKD and CVD mean we have to get […]
Stratifying stroke risk to guide treatment in patients with non-valvular atrial fibrillation
Antiplatelet (usually aspirin) and anticoagulant (usually warfarin) treatments are available to reduce the risk of stroke in patients with atrial fibrillation (AF) but both have potentially harmful adverse effects and warfarin can be time-consuming and expensive to monitor. Guidance exists for choosing between treatments but is often insufficiently detailed to support an informed choice about the risk and benefits. Prescribers and patients are often left with a choice between aspirin or warfarin, and aspirin – which is perceived to be safer and easy to use – is often chosen. This article explores the evidence for aspirin and warfarin in preventing stroke in patients with AF, and describes how we should change the way that decisions about treatment are made.