Quality is the latest buzzword in healthcare. The latest GMS contract emphasises this in the Quality and Outcomes Framework (QOF) designed to measure and reward key elements of primary care chronic disease management. In this issue of BJPCN we start a new series – Points mean Prizes – on how to make sure you get all the ticks in the boxes for the data you need to collect to get maximum QOF points. The series will provide a step-to-step guide on how to score on the 76 quality indicators in the 10 clinical domains of care.
Measuring BP at home
Most people with hypertension are diagnosed and managed on the basis of blood pressure (BP) measurements taken by healthcare professionals in the surgery. Although clinic readings remain the accepted method of measuring and monitoring BP, they are widely acknowledged to be prone to inaccuracies, such as the infamous ‘white coat effect’ that can lead to artificially high readings. In addition, the relatively small number of readings generally taken in the clinic offers only a ‘snapshot’ look at BP levels that may not reflect real values. There is increasing evidence that the use of self BP measurement – with patients monitoring their own BP at home – may provide some advantages over BP measurement in the clinic or surgery. These include potentially more accurate readings and average values that are more reproducible and reliable than traditional clinic measurements. In this article we look at the evidence for the use of home BP monitoring and the accuracy of home monitors.
What to tell your patients about statins
An increasing number of patients are prescribed statins because of the growing evidence that they can dramatically reduce cardiovascular events. However, the withdrawal of one statin – cerivastatin – some time ago may have made some patients concerned about their safety. What should we be telling patients about the benefits of statins, how long they should take them for and whether there are any risks with these widely used agents?
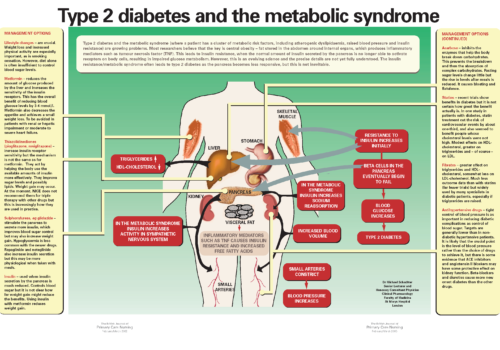
Back to Basics: Type 2 diabetes and the metabolic syndrome
Type 2 diabetes and the metabolic syndrome (where a patient has a cluster of metabolic risk factors, including atherogenic dyslipidaemia, raised blood pressure and insulin resistance) are growing problems. Most researchers believe that the key is central obesity – fat stored in the abdomen around internal organs, which produces inflammatory mediators such as tumour necrosis factor (TNF). This leads to insulin resistance, when the normal amount of insulin secreted by the pancreas is no longer able to activate receptors on body cells, resulting in impaired glucose metabolism. However, this is an evolving science and the precise details are not yet fully understood. The insulin resistance/metabolic syndrome often leads to type 2 diabetes as the pancreas becomes less responsive, but this is not inevitable.
Aspirin in patients with diabetes
Patients with diabetes are at high risk of cardiovascular disease and aspirin is an important part of prevention strategies. Although it is effective and relatively well-tolerated, studies have shown that many patients with diabetes are not taking aspirin. In this article, we review why aspirin should be considered in patients with diabetes, the benefits it might achieve and areas where caution is required.
Making sense of the Quality and Outcome Framework of the new GP Contract
The Quality and Outcome Framework (QOF) of the new GP Contract will be the biggest experiment in improving the quality of care for patients anywhere in the world. By April 2005, we will see how well Primary Care can deliver. In this series, we provide a step-by-step guide on how your practice can get QOF points, including practical information on what data to collect and how to record it. Over the coming months, we will be discussing the best ways to maximise the quality of care and will concentrate on the cardiovascular and diabetes elements of the QOF. We will discuss the setting up of registers, practical tips, examples from practices that are delivering well, how to check how well you are doing from your own IT system and from Quality Management Analysis System and, of course, how to deal with exception reporting and the PCT QOF visit.
Oily fish and cardiovascular disease
The management of cardiovascular disease (CVD) in primary care has been transformed in recent years, particularly with extensive use of statins in secondary prevention. But what about the less high-tech approach of getting patients to eat more healthily? Dietary advice has traditionally been offered primarily to those needing to lose weight or lower their lipid levels. But more recently, systematic reviews have shown good evidence that dietary changes can reduce mortality and morbidity in addition to modifying some risk factors in patients with coronary heart disease. Evidence to date suggests similar benefits of healthier eating are likely in primary prevention. In this new series – Food for Thought – we sort the wheat from the chaff when it comes to dietary advice for patients with cardiovascular disease. This article will focus on the benefits of oily fish, with the good news that simply increasing oily fish intake achieves major benefits.
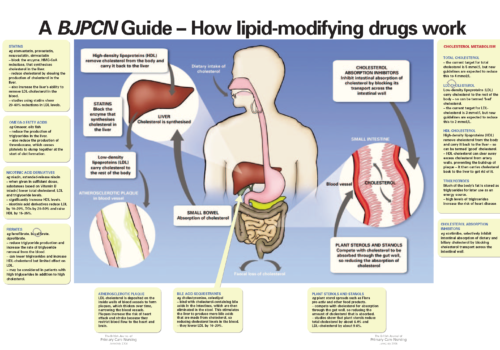
Back to Basics: A BJPCN Guide – How lipid-modifying drugs work
Improving the management of diabetic foot conditions
Foot complications are very common in patients with diabetes. At least one in six diabetics develop foot ulcers at some point in their lives. This article reviews why foot complications occur in diabetes, how you can detect foot problems early, and treatment and prevention strategies. The National Service Framework for Diabetes suggests that targeted foot care for people at high risk could save hundreds of amputations a year. By detecting complications earlier, we can make a real difference to patients’ lives, reducing morbidity, improving quality of life and even saving limbs.
Optimising lipid levels: looking beyond LDL-cholesterol
Treatment with statins is undoubtedly making a major contribution to reducing high-risk patients’ chance of a heart attack or another coronary event. However, their risk remains high, since over half of patients included in statin clinical trials suffered a further coronary event within five years. There is growing evidence that we need to move beyond simply lowering low-density lipoprotein cholesterol (LDL-C) and optimise the whole lipid profile.
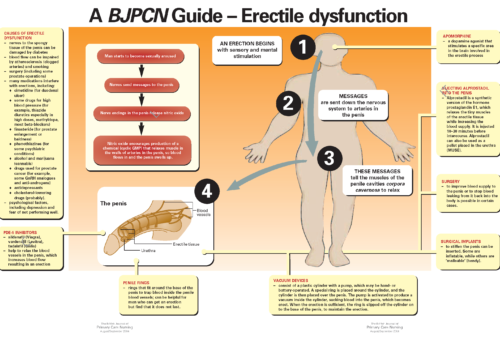
Back to Basics: A BJPCN Guide – Erectile dysfunction
Non-statin strategies for modifying lipids
Raised cholesterol is the commonest risk factor for CHD. Reducing cholesterol can be an effective way to help lower a patient’s risk of heart disease, particularly when cholesterol levels are already high. Dr Rubin Minhas looks at how to help patients to lower their cholesterol levels without drug treatment. He will discuss other lipid modifying drugs in future issues.