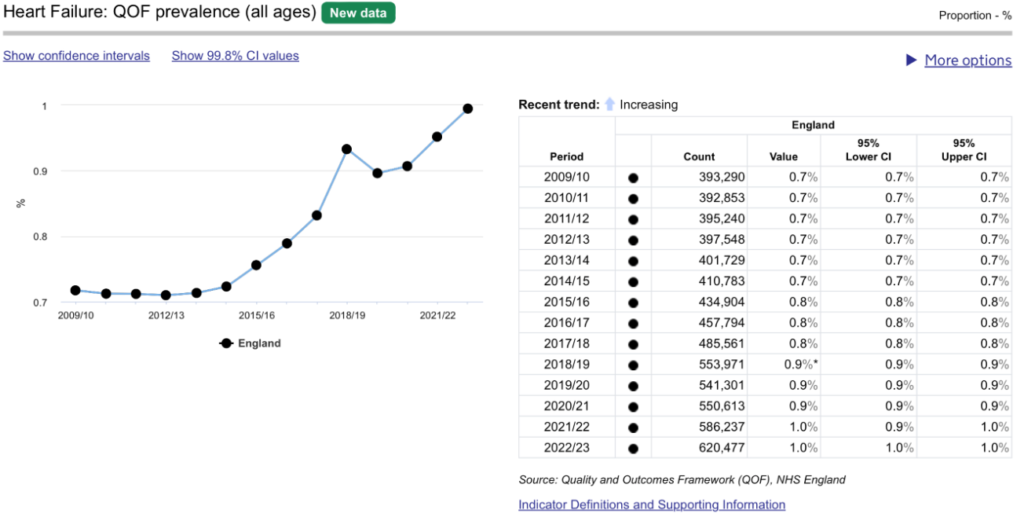
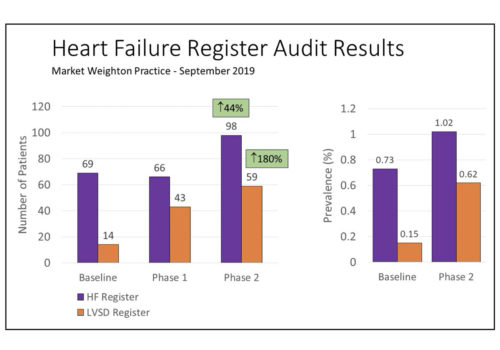
A review of 600 patients notes across a PCN produced an immediate increase in QOF income of over £20k, with the biggest increase in income for indicators HF003 to HF008. Better capture of echocardiogram results and accurate coding of these existing results produced the financial gains. The more comprehensive registers across the PCN will allow improved patient care and patient safety, through recall, clinical review and medication optimisation.
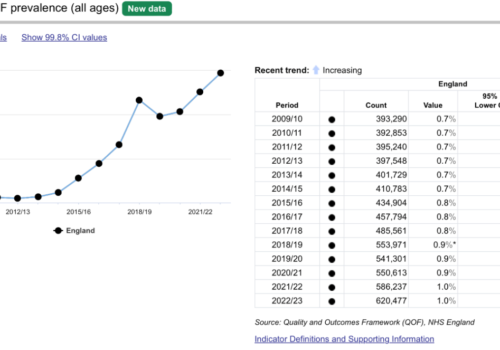
Back to Basics: Respiratory drugs
There are several different drug types used in the management of hypertension. This back to basics provides a useful summary of the different antihypertensive drug classes and how they act to regulate blood pressure.
Multiple sclerosis in primary care – diagnosis and early treatment
What is Multiple sclerosis? Multiple sclerosis (MS), a progressive neurodegenerative disease which arises when the immune system mistakenly attacks and damages tissue in the central nervous system (CNS). This inflammation can affect different sites of the body at different times, producing a wide range of signs and symptoms.
Practical Obesity Management
Recognition of the diverse areas of the brain and multiple neurochemicals and hormones involved in regulation of appetite, satiety and metabolism helps to explain why obesity treatment needs to be individualised and is more complicated that merely instructing people who are living with obesity to eat less and move more. On the contrary, it requires […]
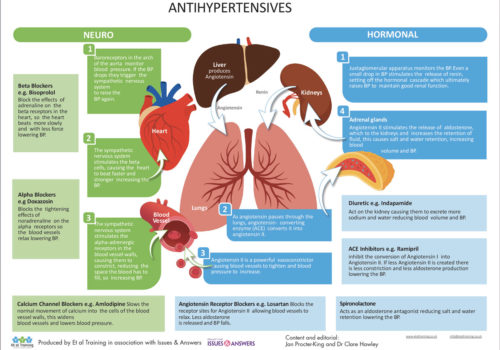
Back to Basics: Antihypertensives
There are several different drug types used in the management of hypertension. This back to basics provides a useful summary of the different antihypertensive drug classes and how they act to regulate blood pressure.
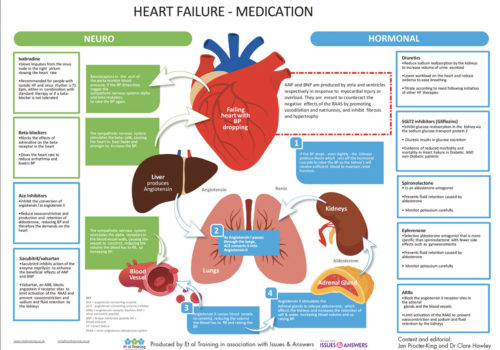
Back to Basics: Heart failure medication
A number of drug classes are used in the treatment of patients with heart failure. This illustrated Back to Basics infographic describes the various drugs and their mechanisms of action to give health care professionals and their patients a greater understanding of heart failure management.
An audit in general practice – Getting a GRASP on heart failure
This audit was carried out using the GRASP-HF audit tool developed by PRIMIS designed to help busy practices achieve a systematic approach to the identification, diagnosis and management of patients with HF.
Freedom from failure – The F word
Nobody likes to talk about failure. We hide from it, shy away from it. Society demands positivity. And so, we do not necessarily take the time or put the effort into learning from failure. Heart Failure is a misunderstood and misdiagnosed condition, as malignant as some of the most common cancers, it should be treated with […]
Impact on mental health – From celebratory ‘Year of the Nurse’ to COVID-19 in 2020
How can nurses be better mental health advocates for their patients and colleagues during the pandemic? 2020 was designated by the World Health Organisation as the inaugural International Year of the Nurse and Midwife. The Covid-19 pandemic has highlighted the critical role nurses play in caring for the mental health of their patients and communities. This article […]
Case study: The hypertensive patient
Working with patients who are not willing to engage fully with healthcare services is a common occurrence. The process requires patience and a focus on providing the patient with full information about their condition and then allowing them to make decisions about their treatment. Here, Dr Terry McCormack (GP and Cardiovascular Lead, North Yorks) describes the approach of his practice to a man with hypertension.
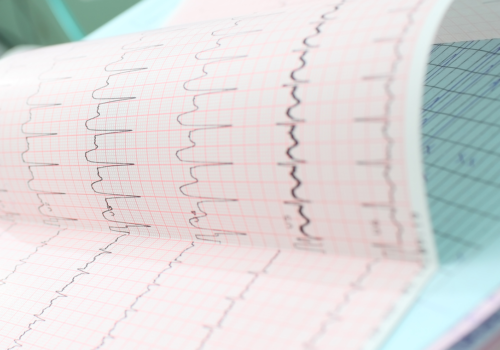
Atrial fibrillation: A closer look
What is AF? Atrial Fibrillation (AF) is the most common heart rhythm disturbance and affects over 33 million people worldwide. Atrial fibrillation or AF occurs when chaotic electrical activity develops in the upper chambers or atria, and completely takes over from the sinus node. As a result, the atria no longer beat in an organised […]
Advice for patients taking ACE inhibitors or angiotensin receptor blockers and coronavirus infection
It has been suggested Hypertension (high blood pressure) may be associated with increased risk of death in hospitalised Coronavirus infected subjects. On non-medical social media sites and some newspapers it has been suggested that commonly used drugs ACEi (ending in ‘pril” e.g. ramipril, lisinopril, perindopril) and ARBs (ending in ‘sartan’ e.g. losartan, candesartan, valsartan) may […]